National Health Center Week (NHCW) 2021, hosted annually by the National Association of Community Health Centers (NACHC), focuses on all the little elements that make our communities stronger. So we decided to run with this theme in celebration of NHCW and educate on how Remote Patient Monitoring (RPM) can support communities across the nation. Jump to this year’s specific focus days, click the shortcut links below:
To see all content related to NHCW week, click here.
National Health Center Week Background
“The Chemistry for Strong Communities,” the theme of this year’s event, pays homage to elements such as Values, Population, Enabling services, Services, Innovations, Affordability, and Mission
Each day of NHCW is devoted to an area of focus, aptly called “Focus Days.” Community health center efforts are integral to all these focus areas and the people they affect. There’s one binding element in particular that can help strengthen health centers and their communities: Remote Patient Monitoring (RPM). RPM is a transformative tool that improves access and quality of care that benefits patients, providers and stakeholders alike. Here’s how RPM affects and/or helps each of the NHCW domains.
Sunday 8/8 Public Health in Housing Day:
Kicking off the celebratory week, this day is devoted to addressing social determinants of health (SDOH), which are “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life, including social, behavioral and environmental determinants of health.”
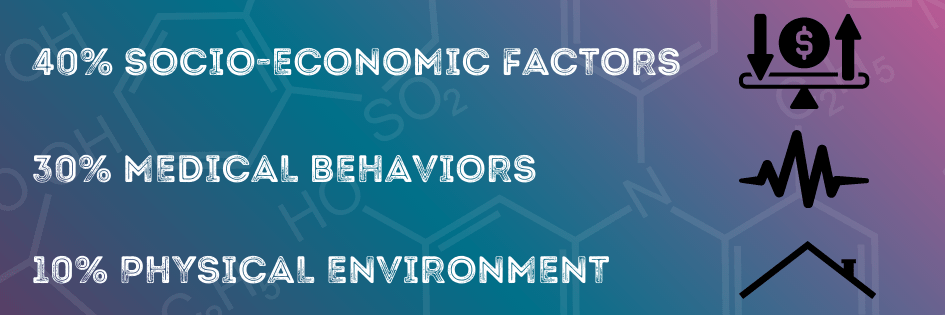
One of the biggest ways to combat negative social determinants of health is to use data and give it context. Medical care only accounts for 10-20 percent of health outcomes. The other 80 percent is influenced by SDOH, which breaks down as:
The key to an effective intervention strategy, this article by HealthcareItNews says, is to enhance patient engagement outside of traditional care venues.
“Services delivered in the home and in the community that address environmental issues like housing, income, crime, education, transportation, domestic circumstances and food insecurity have been shown to improve health outcomes and reduce the cost of care,” the author of the article states.
Read more on this topic: The SDOH Care Gap
The article goes on to say that providers can use SDOH data to be proactive and identify high-risk and vulnerable patients before a health issue occurs. The same is true of RPM data. Eventually, SDOH data can become integrated with RPM data and give the provider a full picture of the situation: physically and socially. Coordinated care efforts can then engage patient- provider- and community-based services to alter care plans for these patients.
“SDOH interoperability requires a framework to identify, measure, and activate social risk factors,” the author continues. “To that end tools like artificial intelligence, natural language processing, patient matching and unique patient identifiers, telemedicine, remote patient monitoring and self-care, records management and algorithms can facilitate the ability to engage and track at-risk individuals across a diverse set of healthcare stakeholders and community-based touchpoints.”
RPM can be a great starting point for launching SDOH data-driven initiatives, and easy to start.
Monday 8/9 Healthcare for the Homeless Day:
“It’s really necessary that people be taken care of where they are,” said Daniel Lam, MD, as quoted in this mHealthIntelligence article. For individuals experiencing homelessness, this rings ever more true. Lam is the director of inpatient and outpatient palliative care services at Harborview, a medical center that has launched a unique program for its patients experiencing homelessness.
The program at Harborview is mobile-health based. It connects patients with Medicare or charity-funded services, such as chronic care treatment, while using a mobile care coordination team. Since the launch of the program, Harborview has seen a 25 percent reduction in ER visits and halved hospital stays for patients treated for at least six months. The program allows patients to be met where they are, rather than waiting for them to seek out a venue of care, which is often the ER.
RPM offers a similar service to help this underserved group of patients. RPM tools can collect data on a regular basis and be sent automatically to the provider, who can then take appropriate actions depending on the severity of vitals. Further advancements could allow Lam’s patient population to one day wear a simple smartwatch that provides pre-identified outcome measures help Lam’s team save time and money (ie. travel costs). This also allows the patient to monitor their vitals themselves, engaging them and prompting them to more closely follow warning signs of deteriorating health. Although RPM is a CMS reimbursable service, more policy changes need to come into effect to fully allow patients experiencing homelessness the freedom to reach out to providers without worry or delay. We believe NHCW is the perfect time to advocate for more patient-centered and proactive solutions such as this one.
Read more on this topic: Mobile Health Care for the Homeless
Tuesday 8/10 Agricultural Worker Health Day:
In another case study cited in mHealthIntelligence, a health system in California is using RPM to improve the lives of agricultural workers and their families. Ag workers often have the least amount of access to quality health care. Livingston, the health system mentioned, has launched a program called ACTIVATE (Accountability, Coordination and Telehealth in the Valley to Achieve Transformation and Equity) in California’s Central Valley. The region was named one of the least healthy in the state. ACTIVATE seeks to improve access for these agricultural communities, as well as encourage adoption of connected care services among patients and providers. 
To help this group of underserved patients, Livingston will provide telehealth and RPM services to patients, as well as furnish them with the technology and education needed to see the services through.
Read more on this topic: Serving Ag Workers Virtually
Not only will ACTIVATE increase accessibility and connectivity for these patients, it also presents an opportunity to build tailored messaging and care. Numbers are objective, yet personal. The data aggregated through RPM is unique to each individual. When services such as health coaching are used in conjunction with RPM, patients can work to understand trends in their data and pinpoint what might be causing issues. This engagement can lead to higher levels of health literacy, which is critical for advancing any health outcomes. When ag workers already live under such different conditions than many of us, a tailored approach to care can help them make health decisions that fit in with their lifestyle, rather than one we see through our own lenses.
RPM is something clinicians can launch within days with the right partner, but ACTIVATE will also be launching a roadmap, in partnership with the Center for Connected Health Policy, for any clinicians wanting to see the efficacy behind the program first. If you’re ready to see RPM in action, click here.
Wednesday 8/11 Patient Appreciation Day:
One of the best things providers can do to show patient appreciation is to validate their concerns and relieve distrust. Patients who mistrust under report health concerns, as explained in this Patient Engagement HIT article. This, in turn, could skew data analytics and lead to inconsistent population health management. Conversely, data presents an opportunity to engage in transparency with patients.
When discussing the future of virtual care, patient comfortability can’t be ignored. In a 2017 Black Book survey, researchers found that 57 percent of health care consumers were skeptical of health IT, with the main concern surrounding health data security. Patients were afraid their data would be shared with third-parties, such as governments and employers. As a result, patients underreported their health conditions and withheld information. Researchers found that 89 percent of patients withheld their health data from their provider because of these privacy concerns. This is worrisome because it brings into question the reliability and usefulness of patient health data.
However, RPM can help fix this problem in two ways. RPM can help providers identify health concerns, even if the patient is underreporting them. The provider can then use this data to be transparent with the patient about their data, who has access to it and how to navigate it. Providing patient education, as mentioned above, increases health literacy, which allows patients to feel more comfortable engaging and advocating for their health. This rapport and consistent engagement can allow patients to gain trust for their providers, as any care interaction becomes a two-way conversation, rather than a lecture. For clinicians who may not always have the time, health coaches are a great substitute for a person who can give patients a walkthrough of what’s happening in their health spheres.
The article cited above also mentions that patients were hesitant of virtual care services due to lack of knowledge surrounding the function of technologies, such as patient portals. Researchers found that, often, these patients were not being taught how to work these portals either. That’s why clinicians can show appreciation for their patients by providing them with services that help give them full understanding of their health situations.
Thursday 8/12 Stakeholder Appreciation Day:
Stakeholder appreciation day seeks to engage legislators and legislative staff who give bipartisan support to community health centers. Health centers often engage with these entities to showcase their efforts and garner more support. One of the best ways health centers can demonstrate the value of the work they do is through numbers. Data can’t lie; it is concrete and undeniable. By implementing a care management system such as RPM, health centers can aggregate that data over time, and hopefully show improved patient outcomes. Systems such as these can simplify intake for stakeholders and allow them to partake in more efficient decision-making.
“Involving stakeholders during all stages of a care management program can lead to early buy-in, successful program design, and establishment of long-term support for the program,” says this guide by the Agency for Healthcare Research and Quality (AHRQ). The agency recommends a few steps for securing support for a new service, such as RPM.
- Identify Champions to assist/support with program rollout and expansion
- Communicate regularly about program successes, failure and new initiatives
- Manage expectations and consider what outcomes stakeholders will find most meaningful
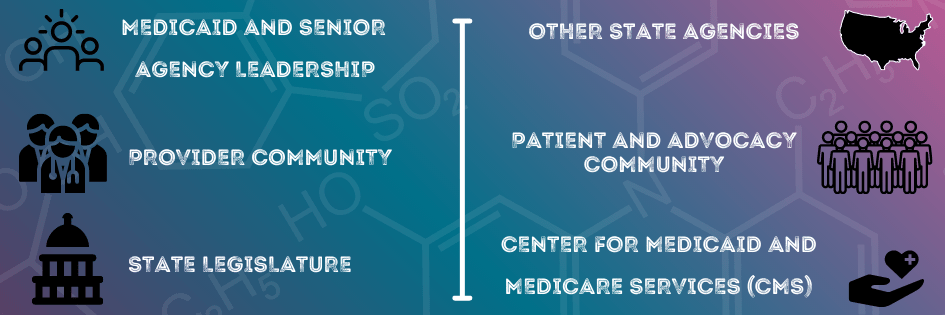
Key groups health organizations should engage to maximize program efficacy include:
To see the complete AHRQ guide to engaging stakeholders, click here.
Friday 8/13 Health Center Staff Appreciation Day:
This day is about thanking health center staff for the commitment and diligence they show in their work. The introduction of new services and workflows can be difficult for some to adapt to. Health center leaders can show appreciation for their staff by collaborating with them when designing new workflows, rather than dictating. Before implementing any new workflows, be sure to ask individual staff members opportunities or concerns they see in the proposed workflow. Opportunities like these can lead to innovation and concerns can help avoid setbacks. Being proactive about both of these opinions can help reduce hesitation and increase comfort.
Obviously, you want to make sure the workflow in question will provide benefits in multiple aspects as well. RPM has been proven to ease workflows by automating processes and decreasing administrative load. Now, about two-thirds of America’s health care systems are taking steps to implement this practice, states this Chief Healthcare Executive article. If this is something that interests you, Harris County Medical Society (HCMS) of Texas has an eight-step process for implementing RPM, which is highly beneficial for clinicians to follow:
1) Identify a need/Establish a patient base
This is the opportunity to ask your staff those aforementioned questions about comfortability and/or hesitation. This can also be a chance to ask your patients what gaps in care they experience. Those who see one can be great customers for RPM beginnings.
2) Form the team
Consider organizing individuals into teams.
-Core (project management team)
-Leadership (key stakeholders)
-Advisory (staff and patients)
-Implementation team (administration and management staff)
3) Evaluate the vendor
The same Chief Healthcare Executive Article recommends asking the following questions when choosing a vendor:
- Does the chosen RPM solution provide support for multiple diseases?
- Does the chosen RPM solution provide a continuous feedback loop in real-time (as required per CMS)?
- Does the chosen RPM solution support EHR integration to facilitate the process rather than complicate it?
- Does the chosen RPM solution have embedded clinical decision making support?
4) Contract with RPM vendor
5) Design a practice workflow with one provider who can commit
6) Prepare the care team with a realistic training environment
7) Partner with and educate the patient (which can be done through a partner like Certintell)
8) Implement RPM and track progress
9) Scale RPM
To see the full HCMS guide with detailed explanations, click here.
Saturday 8/14 Children’s Health Day:
Children are among the most vulnerable patients a health center cares for. The future of children’s health equity warrants innovation. Pediatric RPM is not as integrated into practices as it is for adults, however RPM represents a forward-thinking opportunity for pediatric practices alike. Children’s Hospital network has implemented a RPM pilot program across their practice, that uses RPM in a variety of domains. The goal of the program is to increase health equity for families who are not able to travel long distances to see specialized or general care providers.
The specialties at Children’s using RPM include:
- Enterprise Care Management (ECM) for Medically Complex Patients: This program aims to decrease ER visits and readmissions due to exacerbation of chronic conditions by giving the ECM’s navigator team the ability to deliver care in non-traditional settings.
- Complex Care: This program provides the ECM’s complex care team the same capabilities as stated above
- ACO ED Transitions: This program aims to decrease care delivery costs and decrease the risk of readmission in ED by providing virtual care
- ACO IP Transitions: This program aims to do the same as stated above, but in inpatient departments
- Pulmonary: This program aims to decrease readmissions and costs by allowing the remote monitoring of patients recently discharged from a facility accompanied by a trach/vent.
- Center for Cancer and Blood Disorders: This program aims to give children who have recently been diagnosed with cancer their power back. Through a cellular phone, the patient can receive resources, such as general education, daily care instructions and an electronic ER “fast pass.”
- Post Bariatric Surgery: This program aims to decrease readmissions due to noncompliance for patients who have recently had bariatric surgery.
Certintell Supports YOU During NHCW and Every Day
Whenever you need support, whether it be this week or the next, Certintell has your back. We can provide you with the tools, resources and patient education to start or scale your RPM program within days. To fully integrate proactive, patient-centered care into your practice, we also offer you a suite of other care management services that are easy to integrate into workflows. Our health coaches and network of specialty physicians can alleviate the workload burden from your clinic, so you can focus on imagining an electrifying future for your community. Think we’ve got chemistry? Contact us today!
