Six in ten Americans have at least one diagnosed chronic condition, and 4 in 10 have two or more¹. Many of these diagnosed patients are also Medicare beneficiaries, who compose some of the heaviest users of health care services. These vulnerable patients could also be a part of an FQHC population. What many health care professionals are realizing is that without thorough, tailored and educationally-influenced care, many of these patient’s conditions cannot improve, and can often worsen. Principal Care Management (PCM) is a way to improve the health of these patients with one chronic condition, or one that poses a great risk of deteriorating health.
Chronic conditions can lead to a range of costly complications, such as stroke, nerve damage, loss of vision, heart attack, kidney or liver failure, and mental health conditions. Take for example that 60 percent of the cost of diabetes care can be attributed to potentially avoidable complications and hospitalizations.¹
This is where Principal Care Management can be transformative. At its core, PCM is similar to Chronic Care Management (CCM). However, unlike CCM, PCM’s goal is to develop a care plan that targets one specific high-risk chronic condition. Not only can targeting one condition give a more complete care service, it can also help instill healthy habits in patients, which, in turn, can have a domino effect on adopting more health-conscious choices.
CMS has now authorized FQHCs and RHCs to bill for PCM in 2021. Here’s the main requirements FQHCs should know if they want to take a step up for their patients in the new year.²
Base Codes: HCPCS G2064 (for use by physicians and non-physician practitioners
HCPCS G2605 (for use by clinical staff) ³
| Requirement | Description |
|---|---|
| Time Requirement: | 30 minutes per month |
| Billing Practitioner: | Specialist |
| Necessitated By: | Worsening of condition or hospitalization |
| Intended Length of Time: | Until Condition Improves (Short-Term) |
| Qualifying Conditions: | There are no specific conditions required, but the condition must last:
|
| Care Plan: | Disease-specific |
| Initiating Visit: | Required, can be Annual Wellness Visits (AWV) or other appropriate service |
| Supervision: | General Supervision is permitted during PCM |
| Consent: | Must be obtained before initiating the service and also be documented in the patient’s medical record. |
Other points to note:
- PCM is not necessarily limited to patients with only one chronic condition. Different conditions can be treated and billed by different specialists
- PCM can be billed simultaneously with RPM
- CMS stated the following when it first introduced PCM:
“We are convinced by stakeholders who stated that RPM services are distinct from PCM and could be billed concurrently by the same practitioner for the same beneficiary provided that the time is not counted twice. We will also be monitoring billing of these services.”⁴
- PCM cannot be billed in the same month as CCM
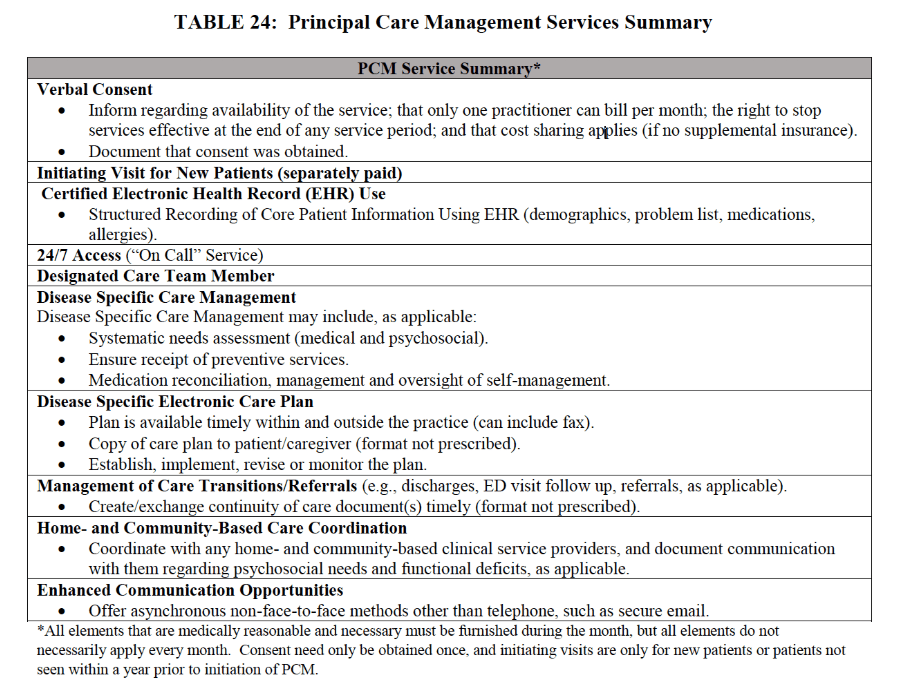
Here is a summary of other PCM requirements from the 2020 CMS Physician Fee Schedule⁵:
Have questions on how to get started? We’re always here if you want to learn more. Certintell is your partner to help you navigate new and complicated care opportunities. We work with you to simplify them, so you can focus on doing what’s most important, while ensuring the same level of care for your patients.
SOURCES:
¹ Holbert, Tony. “The Burden of Chronic Diseases and Their Complications.” Grand Rounds, 14 Dec. 2018, grandrounds.com/blog/burden-chronic-diseases-complications.
² “2021 Physician Fee Schedule Final Rule Released |.” National Association of Rural Health Clinics, 3 Dec. 2020, www.narhc.org/News/28660/2021-Physician-Fee-Schedule-Final-Rule-Released.
³ “Principal Care Management (PCM) Services G2064, G2065.” CodingIntel, 16 Nov. 2020, codingintel.com/principal-care-management-pcm-services-g2064-g2065.
⁴ Orb Health. “2020 CMS Code Updates: Principle Care Management (PCM).” Orb Health, 20 Oct. 2020, orbhealth.com/2020-cms-code-updates-principle-care-management-pcm.
⁵ O’Connor, Kaitlyn. “Principal Care Management (PCM) Reimbursement under the 2020 Medicare Physician Fee Schedule.” Nixon Gwilt Law, 3 Dec. 2019, nixongwiltlaw.com/nlg-blog/2019/12/3/principal-care-management-pcm-reimbursement-under-the-2020-medicare-physician-fee-schedule.



