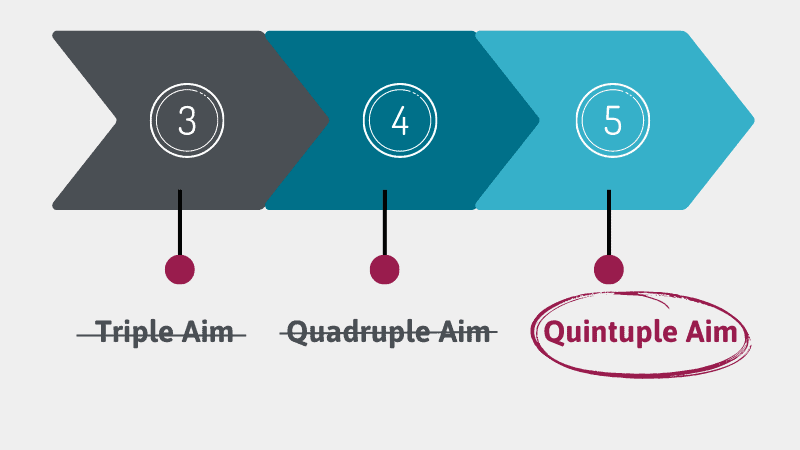
You may already be familiar with the Quadruple Aim, but did you know that healthcare leaders are now moving their focus to the Quintuple Aim to address health equity? The COVID-19 pandemic has brought much-needed attention to disparities that affect the availability of quality and affordable healthcare for marginalized communities. This focus has made many health professionals realize that the Quadruple Aim is missing one essential aspect… health equity.
What Does the New Quintuple Aim Address?
The CDC defines health equity as the state in which everyone has the opportunity to attain their full health potential, and no one is disadvantaged from achieving this potential because of social position or other socially-determined circumstances.¹
Groups that commonly face inequities in the US health system are those who identify as Black, Latino, Native American, and members of the LGBTQ community. Certain geographical areas are also disproportionately affected, including rural areas.
To address these issues, healthcare leaders need to identify existing disparities in their patient populations, implement interventions to address those identified disparities, and measure implemented interventions to determine whether or not they have a positive impact on communities.
In a recent guide, the CDC listed key ways organizations can address health equity in their clinics. The first begins with building organizational capacity to address health equity. Step 1 within this process is establishing an institutional commitment to advance health equity.² Implement this by clarifying and committing to health equity through written promises in your clinic’s mission, vision, and values statement. You can also align funding decisions, recruit staff to advance health equity and integrate health equity into your services and resources.
Let’s go a little bit more in depth into each of those actionable steps, as well as some health IT solutions that can accelerate your health equity efforts:
1. Align Funding Decisions
Before you seek resources, make sure you have a clear understanding of the needs of your community. It’s important that funds are distributed to community partners and other companies that will help promote health equity. By supporting community partners, health systems can share in similar values and visions as the surrounding population, which increases community capacity to produce health equity outcomes. Properly allocated funds can be used to provide health equity training for employees, hire employees from underserved communities, or give funding opportunities to non-traditional partners.²
Recruitment efforts are essential in improving health equity. Employees with diverse skillsets and cultural backgrounds can give a clinic new perspective. Ideally, companies striving toward the Quintuple Aim should try to hire employees from marginalized communities and post job listings in frequently visited areas of the community.
Organizations can also advance health equity through training programs that address cultural sensitivity, and therefore create a more inclusive and emotionally-safe workplace.² The Equality and Human Rights Commission has found that unconscious bias training helps raise employee awareness of disparities they can indirectly cause.³ When employees recognize their unconscious bias, they are more likely to slow down their decision-making process to allow their conscious thought process to make a decision.
3. Integrate Health Equity into your Services and Resources:
Make sure staff is aware of what their expectations are when it comes to implementing health equity in the workplace. What activities should they be participating in to contribute to this goal? To meet the needs of the community, a portion of resources should be allocated to those who have difficulty accessing healthcare services.
The COVID-19 pandemic has challenged and forced our healthcare providers to see how prevalent inequities are in our world, which can no longer go unnoticed.
RPM and telehealth can be great ways to reach populations with limited access to healthcare services. Many patients with health challenges cannot come into the clinic because they cannot take time off of work, find childcare, have a lack of transportation options, or are limited on time. Telehealth provides flexibility in scheduling and requires less of a time commitment, meeting patients where it’s most convenient and therefore reducing many barriers to care. RPM helps patients stay on track with their care plan by allowing their doctors to receive real-time vitals in between appointments. They can then stay up to date on patient status and follow up with patients when vitals are out of range.
Certintell’s RPM solution uses cellular-enabled technology, eliminating the need for wifi connection, which allows patients to access health tools regardless of location or wireless resources. Data obtained from RPM can help investigate patterns, which can highlight disparities. This allows clinicians to have a clearer idea of what intervention is needed for what populations. According to a recent survey, 60 percent of C-suite executives and clinical leaders say that RPM is a critical opportunity for identifying gaps in care and believe it will become the new standard of care over the next two years.⁴
5. Reinforce Health Literacy Programs/Support
Health literacy is essential to a patient’s health. An article from the Academy of Communication in Healthcare discussed the importance of health literacy and patient empowerment. They defined patient empowerment as the patient’s participation as an autonomous actor taking increased responsibility and a more active role in healthcare decision-making.⁵ Health illiteracy is a widespread problem; reports state that 26 percent of Americans achieve inadequate or marginal health literacy.⁵ The article also highlighted that 34 percent of the elderly population enrolled in Medicare have either inadequate or marginal literacy.⁵
Health literacy is essential when it comes to patient self-management. Another research study found that patients with low health literacy had lower health status, which meant less health knowledge, intermediate disease markers and higher measures of morbidity.⁴ It was also found that lower health literacy resulted in lack of preventative services, lower compliance rates, increased hospitalizations, and increased health costs.⁵ The National Institute of Health explains the concept of health literacy as not just being able to read and comprehend health information but it also extends to the ability to understand and navigate materials, challenges, and environments specifically associated with disease prevention and health promotion.⁵ Research on RPM has shown that RPM gives patients greater sense of understanding and autonomy over their care plan, increasing self-management and overall understanding.⁶
How Can Certintell Help
Certintell is a leader in remote monitoring for underserved populations. If your organization is also looking to follow this new era the Quintuple Aim is ushering in, Certintell can work with you and your team to develop a program tailored to your patient’s needs. Whether payer or provider, Certintell innovates solutions for everyone. Contact us today to inquire about our low-cost RPM devices and health data reporting platform with hands-off EHR integration.
SOURCES:
¹ “Advancing Health Equity in Chronic Disease Prevention and Management.” Centers for Disease Control and Prevention, 8 Dec. 2022, www.cdc.gov/chronicdisease/healthequity/index.htm.
² “A Practitioner’s Guide for Advancing Health Equity.” Centers for Disease Control and Prevention, 2013, https://www.cdc.gov/nccdphp/dch/pdf/healthequityguide.pdf.
³ Johnson, Michael. “What Is Unconscious Bias Training for Employees and Why It’s Essential.” Clear Law Institute, 21 June 2021, clearlawinstitute.com/blog/2021/06/07/why-unconscious-bias-training-for-employees-is-essential.
⁴ Schulz, Peter, and Kent Nakamoto. “Health Literacy and Patient Empowerment in Health Communication: The Importance of Separating Conjoined Twins.” Science Direct, 11 Oct. 2012, doi.org/10.1016/j.pec.2012.09.006.
⁵ Siwicki, Bill. “RPM Will Be the New Standard of Care, a New Study Says.” Healthcare IT News, 4 Nov. 2021, www.healthcareitnews.com/news/rpm-will-be-new-standard-care-new-study-say.
⁶ Parthasarathy, Kas. “Addressing Health Equity Through Remote Patient Monitoring and Continuity of Care.” Amazon Web Services, 3 Oct. 2022, aws.amazon.com/blogs/industries/addressing-health-equity-through-remote-patient-monitoring-and-continuity-of-care.